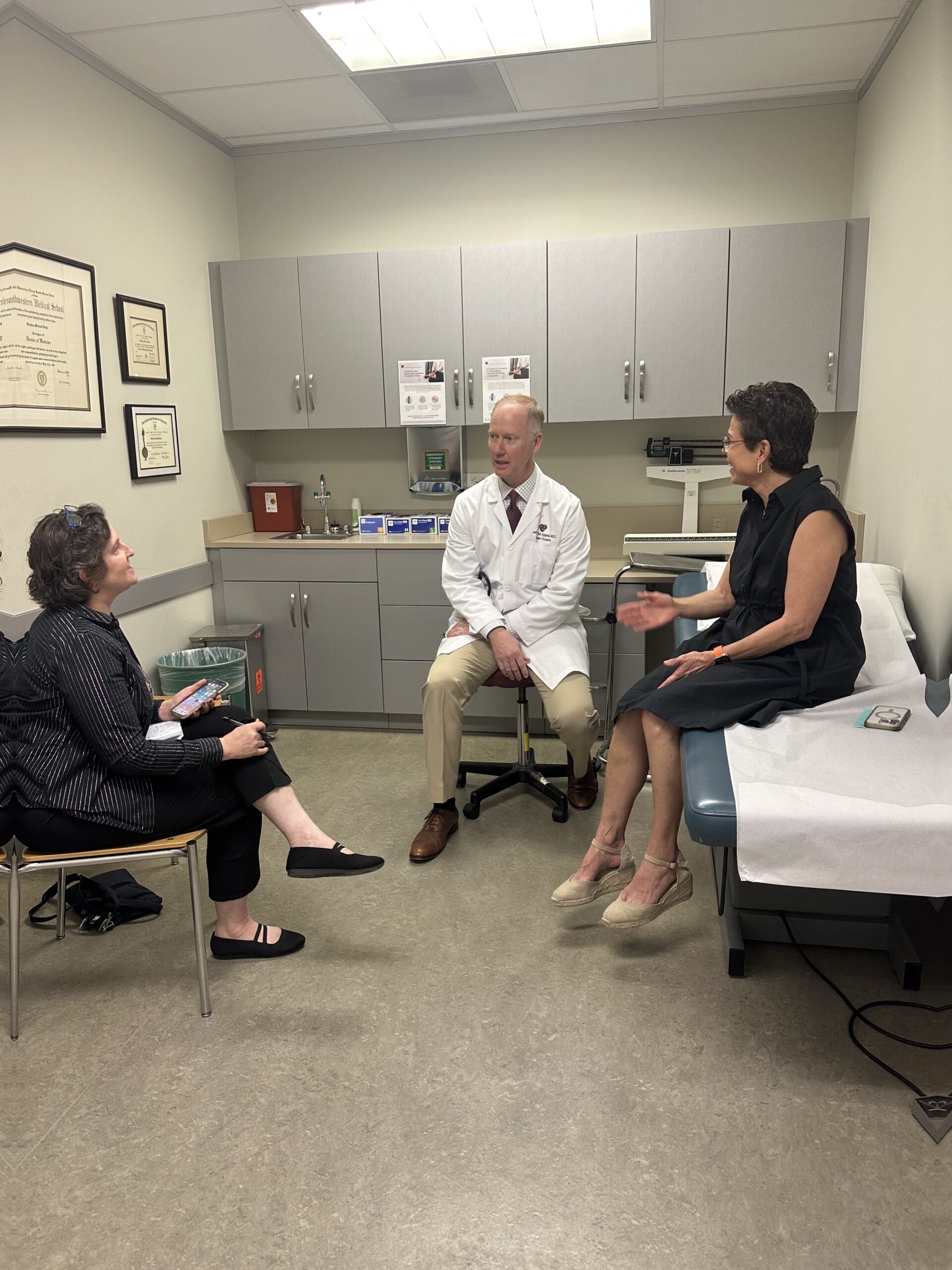
CTVS patient and marathon runner, Alejandra Saitas, shared her stroke survival story with Nicole Villalpando from the Austin American Statesman in honor of Stroke Awareness Month to help educate others about the lesser-known symptoms she experienced that took her by surprise. You can read her story below or find it on the Austin American Statesman website here.
Alejandra Saitas is not who you think of when you think stroke. The 60-year-old Austinite has been running for 30 years, done marathons and half Ironman triathlons. She runs five times a week and lifts weights two days.
Her cholesterol is “perfect,” she says, and she doesn’t need any medication for high blood pressure. She eats a low-sugar, gluten free diet, has never smoked or done drugs and rarely drinks alcohol.
On March 3, when she and husband Jeff were having dinner after finishing the Tokyo marathon, stroke “wasn’t even on my radar screen,” she said. “I was more worried about breast cancer or auto immune disease that runs in my family.”
At dinner, she treated herself to a peach nectar with a little bit of sake. Then as she was talking to her husband, she tilted a little bit and her smile was drooping slightly on one side.
He suspected something was wrong and asked her to lift her arms on top of her head and other motions to see if anything else was weird. “I was doing everything fine,” she said. “In fact, I got mad. I thought, ‘Jeff, I just had a drink. It went to my head. That was a stupid thing to do after you run a marathon. You’re dehydrated. … I’m drunk. Stop with the questions.'”
She started feeling nauseated. Then when she went to the bathroom, her balance was off and she had to have Jeff help her walk to the bathroom. They finished the meal, went back to the hotel and went to bed.
The next day, the Saitases left Tokyo, but at the airport, Alejandra Saitas kept bumping into people and even into a pole. Her peripheral vision was affected. She got on the 13-hour-flight to Dallas and then another flight to Austin, which she now realizes she shouldn’t have done.
Like a meteor shower in her brain
Once home in Austin, she felt fine, but she humored her husband and went that day to the emergency room at the Heart Hospital of Austin.
There a CT scan revealed she had a clot in her carotid artery. The doctors at the Heart Hospital sent her to St. David’s Medical Center, which has a specialized stroke unit. An MRI of her brain looked like a meteor shower, she was told.
Dr. Jeffrey Apple of Cardiothoracic and Vascular Surgeons explains that Saitas had plaque in her carotid artery. A blood clot formed around that plaque, and then part of that clot broke free, went into the brain like a meteor, hit other branches of blood vessels and then spread like a meteor shower in the brain. That clot going to the brain was the stroke.
A growing risk of stroke
The incidents of stroke deaths are expected to increase by 46.83% globally by 2050, according to a World Stroke Organization and Lancet Neurology Commission report. Stroke incidents are also being seen in more younger people, those younger than 55.
While that was a global report, Dr. Farzan Ghodsianzadeh, the director of stroke care at Baylor Scott and White Health, said that in the United States and Texas, the rates of stroke are rising alongside our rates of obesity, high cholesterol, high blood pressure, diabetes, atrial fibrillation (an abnormal heart rate) and our decrease in activity. Access to health care and primary care visits also is having an impact, he said, because people are missing screenings.
Strokes can be caused by either not enough blood going to the brain or too much blood in the brain, Ghodsianzadeh said.
The kind of stroke Saitas had is one that can happen in otherwise healthy people who build up more plaque in their arteries, usually because of genetics, Apple said. When those plaques rupture, “that’s when the problems occur,” he said.
Time is of the essence
Getting to the hospital immediately is the most important thing with strokes, Ghodsianzadeh said, because the new clot-busting medications need to be given within a 4½-hour window of the stroke. A procedure to remove the blood clot also can be done within a short window of the stroke occurring.
“This is the scary thing about strokes,” Apple said. “Once they occur, you really are on a time clock if you’ve had a major stroke. We tell people you have about six hours to really do something that can reverse those changes. … Strokes leave a permanent problem.”
“That’s kind of the major thing,” Ghodsianzadeh said. “Only about 10 to 20 percent of patients are getting there in time.”
Understanding the stroke symptoms
Saitas was among the vast majority of people who didn’t get to a hospital within the recommended window. The symptoms were confusing to her. She knew about facial droop, but hers was slight. She did not have garbled speech; nor did she have uneven use of her arms or legs.
The old memory aid: FAST (Face droop, Arm or leg weakness, Speech problems and Time to go to the hospital) was changed in 2017 because there are a significant number of people who had symptoms outside of FAST.
The phrase to remember is BE FAST.
- Balance (loss of balance, dizziness or headache).
- Eyes (blurred vision, double vision or peripheral vision problems).
- Face (one side of the face is drooping).
- Arms (weakness in an arm or a leg).
- Speech (difficulty speaking or understanding words).
- Time (time to call for an ambulance immediately to get help).
With strokes people often think it is something else, including “‘Oh, I’m dehydrated,'” Apple said. “‘Oh, I have a virus.’ It will kind of sneak up on you.”
Preventing the next stroke
With blood thinners in the hospital and continuing them at home, Saitas’ body dissolved the stroke. The plaque was still in her carotid artery, waiting for the next blood clot. “Its like a quiet or silent volcano,” Apple said. “They cause you no harm when they are quiet, but when they are not quiet, that’s the problem.”
She could have continued on blood thinners for the rest of her life, or she could have a stent put into her artery to secure the blood flow and prevent the plaque from moving from that area.
“I didn’t want her to go back to heavy running until we had covered that plaque with a stent,” Apple said.
On April 19, Apple inserted a transcarotid artery revascularization stent into Saitas’ carotid artery using a catheter. During the procedure, Apple is able to reverse the blood flow so that if any plaque breaks off, it will flow in the direction of the femoral vein and not to the brain. Once the nickel and titanium stent is placed, Apple then allows the blood to flow back to the brain and removes the catheter and guide wire.
For Saitis this was an easy procedure. She just had to sleep with her head elevated for a few days and not run for three to four weeks.
She has a little S-shaped scar on her neck: S for survivor, she says. The scar she says, “I don’t even mind. I am here, alive and I am very grateful.”
She is returning to running, but maybe not doing a marathon again. “Running a marathon at 60 is a little hard,” she said, but she does have her eye on a half marathon next year in New Zealand that is “Lord of the Rings” themed.