What is Peripheral Artery Disease or PAD?
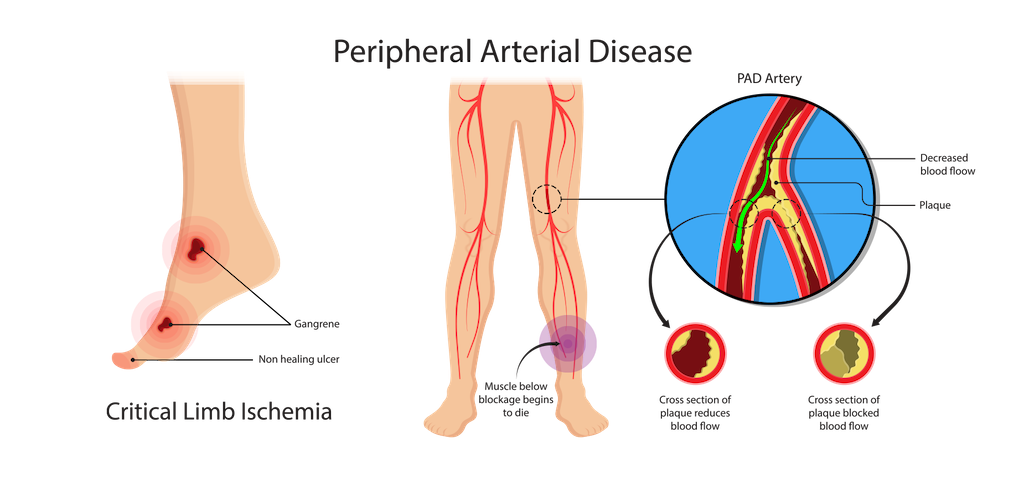
Peripheral artery disease (PAD) is a circulatory condition in which the blood vessels are narrowed causing reduced or blocked blood flow to your extremities. This is usually due to the build-up of fatty plaque in your arteries, and while this can happen in any blood vessel, it occurs most commonly in the legs. The resulting poor leg circulation can lead to excruciating leg or hip pain, non-healing foot or leg ulcers, or even more serious issues like stroke or loss of limbs if left untreated.
According to the Society for Vascular Surgery, approximately 10 million Americans suffer from PAD.
Peripheral Artery Disease Symptoms
Classic symptoms of PAD include pain, cramping, or tiredness in the buttocks, hip, thigh, or calf which starts while walking. Non-healing foot or leg ulcers or wounds are also very common.
Who is at Risk for PAD?
Those with a high-risk factor for developing PAD include people that have:
- Diabetes
- High blood pressure
- High cholesterol
- Atherosclerosis (the hardening or narrowing of your arteries)
- End stage renal disease
Or people who:
- Smoke
- Are older than 60
Walking and PAD
Many patients with PAD do not need medical intervention right away. Learn more about the walking program at CTVS and how regular walking can improve PAD symptoms.
When should you see our PAD specialists at CTVS?
It’s time to make an appointment with one of our board-certified vascular specialists if you experience any of the following situations–some may even require urgent attention:
- Difficulty with walking or pain with walking
- If you have pain or cramping in your calf, thigh, or buttocks when walking and that pain is relieved when you rest.
- Early signs of a threatened extremity
- You notice your feet are cooler in temperature, you develop hair loss or shiny skin on your feet or legs, or have slow growth of your toenails.
- Progressive signs of a threatened extremity
- You develop numbness, weakness, or small ulcers on your toes, feet, or lower leg. These are early signs of tissue death from PAD and you should be seen urgently.
- Severe signs of a threatened extremity
- If you have severe pain in your foot at rest, develop black/darkened toes, or develop severe ulcers. These symptoms require immediate consultation.
What are the Most Effective Treatment Options for PAD?
Diagnostic testing is conducted in our own fully-accredited Vascular Lab where we can obtain measurements of blood flow and how well your arteries and veins function.
Following diagnostic testing, your treatment plan may include one or a combination of the following:
- Medical Therapy – An important part of vascular health is optimizing both your medical therapy as well as your health habits. We work with various healthcare providers to ensure you are on the right medications. In addition, we offer counseling for tobacco cessation and exercise therapy.
- Minimally Invasive Procedures – We can treat patients with PAD using a minimally invasive, percutaneous technique referred to as an arteriogram. We will use balloons, stents and atherectomy devices to restore blood flow to your damaged extremity. These procedures are usually performed conveniently at our own Vascular Intervention Suite (VIS) without the need to go to the hospital.
- Surgical Revascularization – Unlike other specialties, we are certified in open surgical techniques which are better suited in certain situations when less invasive options are not feasible. These include limb bypass (surgery to reroute the blood supply around a blocked artery) and endarterectomy (surgical removal of part of the inner lining of an artery).
- Foot and Leg Wound Care – We work with podiatrists and other wound care specialists to promote wound healing and preserve tissue.
- Amputation – When necessary, our vascular surgeons perform amputations to save patients from life-threatening complications. At CTVS, we have an extensive limb preservation program and perform amputations only as absolutely necessary. We work with you and prosthetic specialists to help you return to your daily activities.
Navigating Life After Peripheral Artery Disease Treatments
Our physicians will give you specific instructions when you leave our office or the hospital about recovery times and returning to work or your regular activities. Depending on your treatment, most patients return to our office within three months to ensure adequate blood flow to your extremity. PAD can be a progressive disease, therefore we like to visit with you at least once a year to prevent any further complications.
Leading the Way in Vascular Care: Introducing Our PAD Specialists
- John Politz, MD, FACS
- Stephen Settle, MD, FACS
- Joe Wells III, MD, FACS
- Scott Seidel, MD, FACS, RVT
- Jeffery Apple, MD, FACS
- Bradley Boone, MD, FACS
- David Nation, MD, FACS
- Ryan Turley, MD
- Taylor Smith, MD, FACS, RPVI
- Nicolas Zea, MD, FACS, RPVI
With state-of-the-art imaging diagnostics and both open and minimally-invasive surgical treatment options, our team of vascular surgeons is able to provide interventions for the full spectrum of circulatory disorders.
Written by: Jeffrey Apple, MD | Last Reviewed 8 Mar 2024
To schedule an appointment or for more information
Call: 512-459-8753
Peripheral Artery Disease FAQs
What is Peripheral Artery Disease (PAD)?
Peripheral Artery Disease (PAD) is a condition that affects blood flow in the arteries outside the heart, most commonly in the legs.
What are the common symptoms of PAD?
Common symptoms of PAD include leg pain, cramping, weakness, and numbness, especially during physical activity.
Are there any risk factors for developing PAD?
Yes, risk factors for PAD include smoking, diabetes, high blood pressure, high cholesterol, and a sedentary lifestyle.
How is PAD diagnosed by your PAD specialists?
Our PAD specialists use a combination of physical exams, medical history reviews, and non-invasive tests like ankle-brachial index (ABI) to diagnose PAD.
What treatment options do your PAD specialists offer?
Our PAD specialists provide personalized treatment plans, including lifestyle changes, medications, angioplasty, and vascular surgery, depending on the severity.
Can PAD be prevented?
Yes, adopting a healthy lifestyle, quitting smoking, managing diabetes and blood pressure, and regular exercise can lower the risk of PAD.
How can I schedule an appointment with your PAD specialists?
To schedule an appointment with our PAD specialists, you can call our office or use the online appointment request form on our website.
