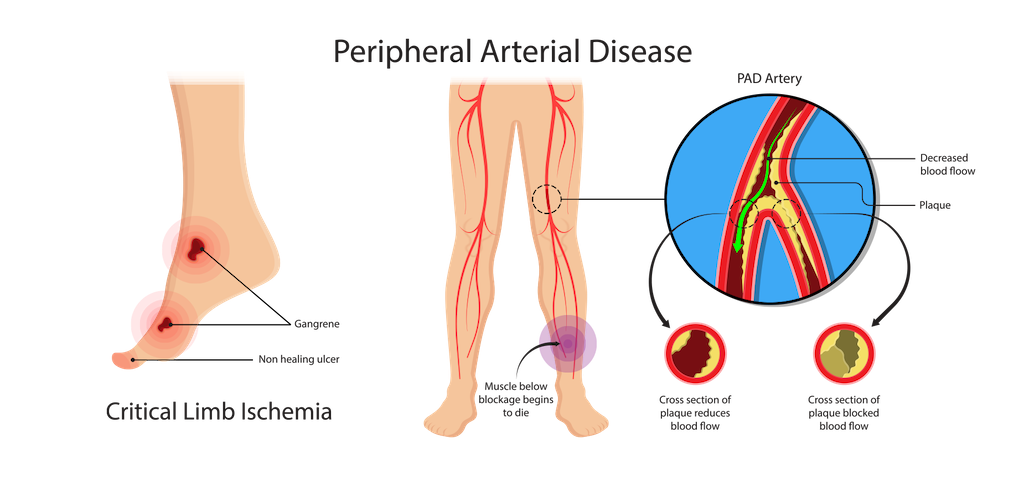
Peripheral Artery Disease (PAD) is a circulatory condition that affects blood vessels and causes reduced blood flow, particularly in the legs. One common complication of PAD is the development of ulcers or open sores that heal slowly or not at all. These ulcers can be painful and may lead to more severe health problems if not properly treated.
The board-certified vascular surgeons at CTVS are experts in diagnosing and safely and effectively treating PAD ulcers and other complications of peripheral artery disease. If you or a loved one are struggling with PAD ulcers, contact us today to schedule an appointment with one of our experienced surgeons.
What Are PAD Ulcers?
PAD ulcers, also called arterial ulcers, are open sores that develop on the skin due to poor circulation caused by conditions like peripheral artery disease. These ulcers typically form on the lower legs, feet or toes, where blood flow is most restricted. Unlike other types of ulcers like venous or diabetic ulcers, PAD ulcers are primarily caused by a lack of oxygen-rich blood reaching the affected tissue. This oxygen deprivation leads to tissue damage, resulting in the formation of painful, non-healing wounds.
PAD ulcers are often characterized by a punched-out appearance with well-defined edges. In severe cases, PAD ulcers may expose underlying structures such as tendons or bones. The skin around the ulcer may appear shiny or pale, and the ulcer itself may be uncomfortable or painful, especially at night.
What Causes PAD Ulcers?
PAD ulcers are caused by the same underlying issues that contribute to peripheral artery disease. PAD occurs when the arteries that supply blood to the limbs become narrowed or blocked due to atherosclerosis, a condition in which fatty deposits, cholesterol and other substances build up on the artery walls. This buildup restricts blood flow, reducing the oxygen and nutrients that tissues need to stay healthy.
Without adequate oxygen, the skin and underlying tissues start to break down, leading to the formation of ulcers. Even minor injuries can trigger the development of PAD ulcers, as poor circulation also compromises the body’s natural healing process.
Risk Factors for PAD Ulcers
Several risk factors can increase the likelihood of developing arterial ulcers:
- Age. Arteries naturally become less elastic and often narrower with age, increasing the risk of developing PAD, particularly over the age of 60.
- Smoking. Smoking is one of the most significant risk factors for PAD and PAD ulcers, as it can damage blood vessels and accelerate the progression of atherosclerosis.
- Diabetes. Diabetes increases the risk of PAD by contributing to the buildup of fatty deposits in the arteries. It also impairs wound healing, making ulcers more likely to develop.
- High blood pressure. Hypertension can damage the arteries and lead to the development of PAD.
- High cholesterol. High cholesterol levels contribute to the formation of fatty plaques in the arteries, reducing blood flow and increasing the risk of ulcers.
- Obesity. Excess weight puts additional pressure on the arteries and contributes to other risk factors like high blood pressure and diabetes.
- Sedentary lifestyle. Lack of physical activity can lead to poor circulation and increase the risk of developing PAD ulcers.
- History of cardiovascular disease. Those with a personal or family history of heart disease or stroke are at a higher risk of developing PAD and PAD ulcers.
Symptoms of Arterial Ulcers
Arterial ulcers most frequently form on the legs, feet, toes or ankles, but they can form anywhere on the body. Common signs to look for include:
- Skin that appears tight, shiny, thin or pale.
- Skin that feels cool or cold to the touch due to poor circulation.
- Reduced or loss of hair growth in the affected area.
- Red, yellow or black sores on the skin that do not bleed.
- A “punched-out” appearance with well-defined edges.
- Wounds or sores that are very slow to heal or do not heal at all.
- Persistent leg pain, which often worsens at night.
Treatment Options for PAD Ulcers
Treatment for PAD ulcers focuses on improving blood flow to the affected area. The best treatment option for you will depend on factors like the size, location and severity of ulcer, as well as other risk factors or complications. After a careful assessment and diagnosis of your condition, our vascular experts will work closely with your care team, which can include a wound care specialist and podiatrist, to create an individualized treatment plan based on your specific needs.
Common treatment methods for arterial ulcers can include:
- Medication. Drugs to improve blood flow, lower cholesterol, control blood pressure and manage diabetes may be prescribed to address the underlying causes of PAD.
- Wound care. Specialized wound care is essential for managing PAD ulcers. This may include debridement (removal of dead tissue), specialized wound dressings and use of topical medications to promote healing.
- Lifestyle changes. Quitting smoking, adopting a healthy diet, getting regular physical activity and managing chronic conditions like diabetes can help to promote wound healing and prevent further complications of PAD and PAD ulcers.
- Revascularization. In some cases, surgical procedures such as angioplasty or limb bypass may be necessary to restore blood flow to the affected area and promote healing of the ulcer.
- Amputation. In severe, life-threatening situations, amputation may be necessary. At CTVS, our vascular surgeons perform amputations to save patients from life-threatening complications and we take all steps possible to achieve amputation prevention.
When to See Our PAD Specialists at CTVS
If you have PAD or are at risk for developing this condition, it is important to make an appointment with one of our board-certified vascular specialists if you notice any signs of ulcers, such as persistent pain, skin changes or slow-healing wounds. Early detection and treatment are key to preventing complications and ensuring the best possible outcome.
Our vascular experts can provide a comprehensive evaluation, recommend prevention strategies and the best treatment methods and guide you in managing your condition to prevent further issues. We are here to provide expert care and help you take control of your health.
Written by: Jeffrey Apple, MD | Last Reviewed 30 Aug 2024
